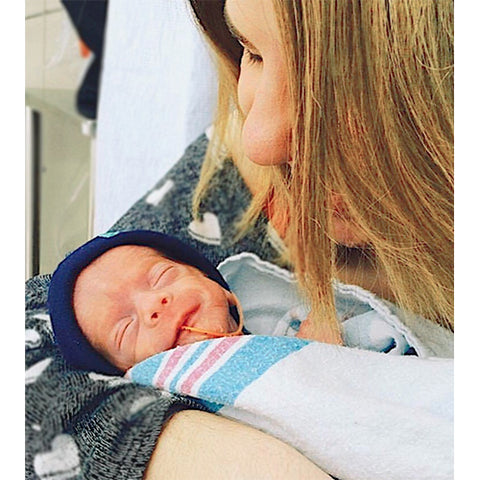
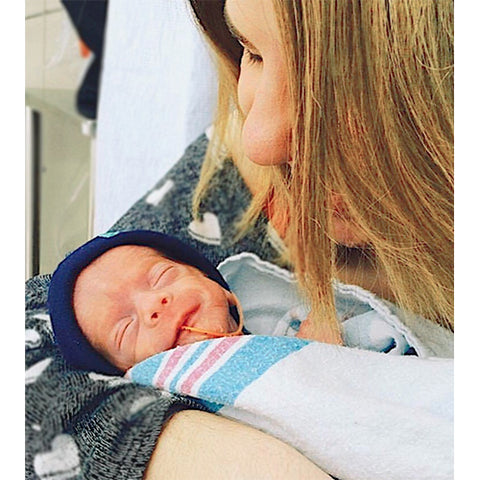
A few days ago, I came across @oneinamulligan on Instagram. The story on her feed inspired me to share it with all of you. She is an amazing young mother, who like so many of us, had a dream of starting a family with the man she loved. Unfortunately, the story was not an easy one. After three years of countless procedures, appointments, and dozens of pregnancy tests, their dream finally came true. In 2016 through IUI, Flynn arrived a little earlier than expected but very LOVED!

Kristina has turned her struggles into a beautiful blog (https://www.oneinamulligan.com/) to help other preemie parents struggling with the same issues Kristen has faced. She has given me permission to share her information packed posts covering so much of what preemies and their parents journey through...
Day One: November is Prematurity Awareness Month. ??
Like last year, I will share parts of our story, facts, statistics, and things to know about all things preemie!
Day Two:
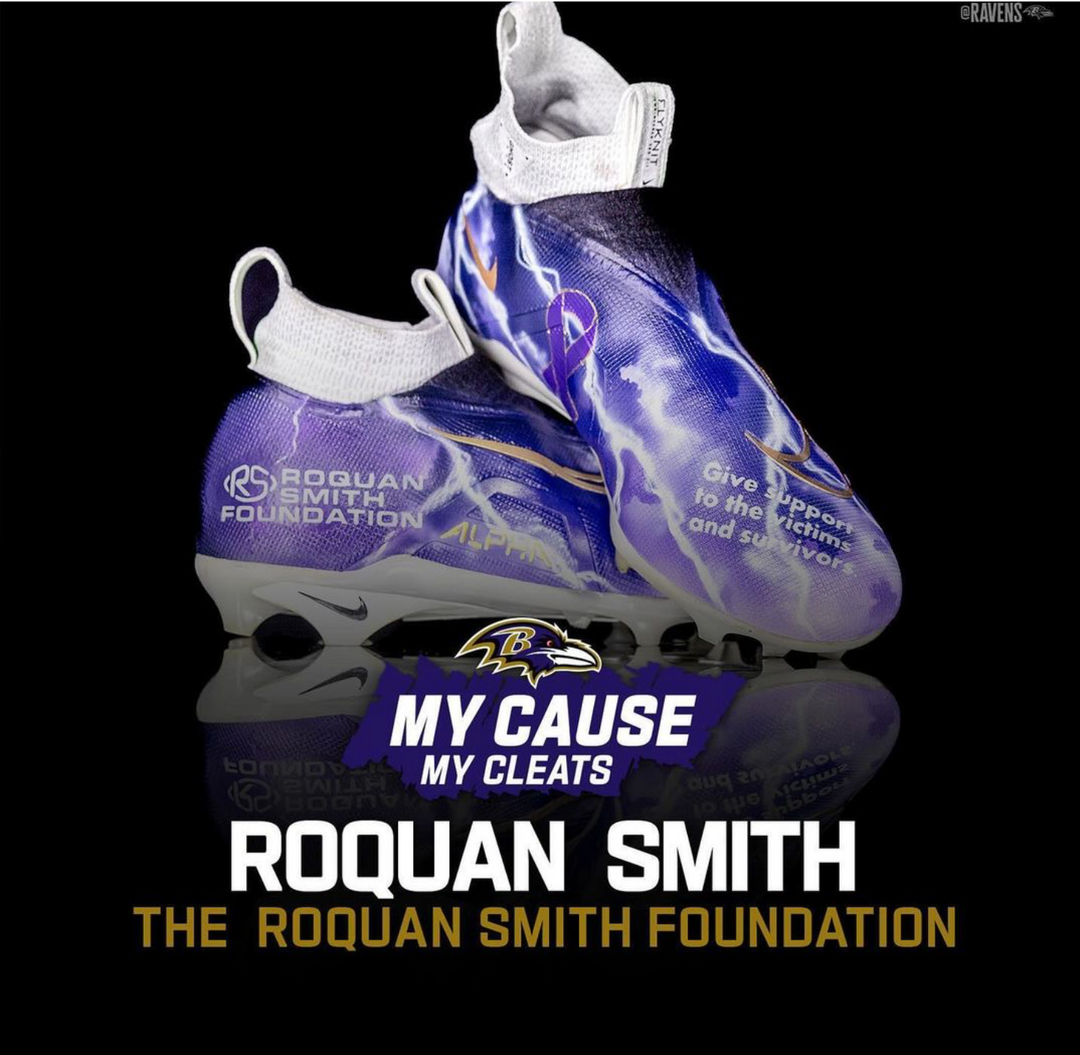
Did you know that purple is the color for Prematurity Awareness Month? The color purple symbolizes both power and magic, so I find that to be a perfect choice.
You will see individuals sporting purple for preemies throughout the whole month of November; on the 17th, you will see purple across the globe for World Prematurity Day - bridges, skyscrapers, and landmarks alike. This widespread support hopefully brings more awareness and hope for a healthy start for more babies everywhere.
Day Three:
How could I raise awareness for Prematurity Awareness Month if I didn't share what that means?
"Preterm" or "premature," as a whole, is any baby born before 37 weeks of the standard 40 weeks of pregnancy. Within this umbrella term, there are different classifications based on gestational age (the number of weeks at the time of birth).
Late Preterm is a baby born between 34-37 weeks.
Moderately Premature is a baby born between 31-34 weeks.
Very Premature is a baby born between 27-30 weeks.
A Micro-Preemie is a baby born before 26 weeks gestation.
If you research and believe me, you will find that credible resources have conflicting thoughts on each category's specifications. Preterm babies' weight is measured using grams, and sometimes there is an overlap in gestational age and weight.
It is essential to classify prematurity levels because, though every child and circumstances are different, each label comes with unique concerns. The general rule is that the earlier the birth, the longer the NICU stay and the more hurdles there may be to overcome.
Day Four:
Let's talk about some hard but important stuff. The things that make raising awareness so integral. Globally, complications due to preterm birth are the leading cause of death among children under five.
Things you should know:
• Prematurity (and its resulting complications) were responsible for approximately 1 million deaths in 2015.
• Common causes of death for premature babies include respiratory distress syndrome (RDS), necrotizing enterocolitis (NEC), and intraventricular hemorrhage (IVH).
• Preterm-related causes account for more than one-third (36.3%) of infant deaths in the United States.
• In low-income areas, half of the babies born at or below 32 weeks die due to a lack of accessible, cost-effective care, such as warmth, breastfeeding support, and basic care for infections and breathing difficulties. This would not be the case if these babies were born into a higher-income setting.
An estimated 15 million babies are born too early every year. That is more than 1 in 10 babies. Worldwide, we have to be better and do better for the 1 in 10.
Statistics from March of Dimes, CDC, and WHO.
Day Five:
Of course, preterm birth has existed since the beginning of time. If babies are born, the risk of prematurity is there, but care as we know it today began right in New York around one-hundred years ago.
It was Coney Island in the early 1900s. Beyond the sword swallowers and other sideshow performances (think the “Four-Legged Woman”) was an entirely different exhibit: rows of tiny, premature babies living in glass incubators complete with carnival barkers encouraging visitors to approach them.
The first Incubators arrived in 1870’s France after obstetricians borrowed the idea from farmers using a similar treatment for baby chickens. The first design was hardly different than hot water bottles and baby blankets, but the concept of keeping babies who cannot regulate their body temperature warm was the same as it is today.
The second generation of obstetricians refined the incubators, adding thermostats and ventilation systems, and spread the word through demonstrations at Worlds Fairs. It was not until
1896 in Berlin that Dr. Martin Couney first saw these machines keeping premature babies alive and began importing them to the United States, specifically to Luna Park on Coney Island.
As you can imagine, the mortality rates of premature babies at this time were too high, and many of the babies in the exhibits came from local maternity wards that could not care for them. Dr. Couney never charged parents for the care he provided, and his daughter (who was born prematurely) even spent time in the exhibit.
Couney always claimed a higher purpose for his exhibits — to show how a great new technology could save fragile children and convince the reluctant medical field to embrace that technology. It was not until after his death in 1950, however, that incubators became common in hospitals. This equipment has advanced over time, and these advancements in science and technology have saved countless premature babies.
The families of babies that were once in Dr. Couney’s care have always acknowledged the powerful impact he had on their lives.
Day Six:
Let’s talk about one of the common causes of premature birth: preeclampsia. I was diagnosed with preeclampsia during my pregnancy, causing Flynn to be born at 28 weeks.
This topic is on my heart today after reading the news about Dr. Chaniece Wallace of Indianapolis. She died just two days after she and her husband, Anthony, welcomed their daughter, Charlotte. Dr. Wallace gave birth to her daughter at 35 weeks and died of postpartum complications caused by preeclampsia.
Preeclampsia is a pregnancy complication characterized by high blood pressure and signs that some of the mother’s organs, like her kidneys and liver, may not normally be working. Usually, this condition occurs after the 20th week of pregnancy or after a baby’s birth. Preeclampsia is often treatable, but in more severe cases, like mine, the only way to treat preeclampsia is to deliver the baby, which is why there is such a prevalent link to premature birth. Health problems for women who have preeclampsia include kidney, liver, brain damage, blood clotting issues, and eclampsia (a rare and life-threatening condition where a pregnant woman has seizures or falls into a coma after preeclampsia), and stroke.
This condition is a severe health problem for pregnant women worldwide, affecting 2-8% of pregnancies worldwide. In the United States, specifically, it is the cause of 15% of premature births.
The cause of preeclampsia is unknown, but some things may make some more likely than others to have it, including obesity, diabetes, personal history of high blood pressure, or family history of preeclampsia. It’s essential to know the signs, including changes in vision, a headache that doesn't go away, vomiting or dizziness, sudden weight gain, and swelling. If you are concerned that you may develop preeclampsia, please voice your concerns to your physician.
Day Seven:
The birth of a baby is an occasion to celebrate, no matter the circumstances, no matter how small. I made the decision, in the thick of it, to cancel my baby shower. The choice, on my part, was made in grief. Just a couple of weeks after Flynn was born, my baby shower date arrived, but I was just too overwhelmed to even think about the rest of the planning needed. I could not even imagine the difficult conversations that would be had that day given our family situation. I didn’t want to talk about it; I didn’t know-how. I didn't want to hear anything that sounded like pity. That is not what I wanted my shower to be.
It turns out that, unbeknownst to me at the time of voicing my decision, I would be in the ICU on the day of my baby shower. My sister and mom took care of everything, canceling all arrangements definitively.
When we called off the shower, it ended the hope of any excitement and celebration.
We were a family with a baby in the NICU, where circumstances and statistics would change each day. Our homecoming as a family of three was not a sure thing, especially given my eventual state. With that, people didn’t know what to say. They didn’t know what to do.
My miracle baby, who had been very long-awaited and strived for, faded into the background. As new parents, we entered into our new life phase without a sound, clinging to each other for hope and celebrating ourselves.
I tell you this so that, if you’ve ever been in these shoes, you don’t feel alone. I’m celebrating with you. If you find yourself facing this situation with someone you love: congratulate them. Throw literal confetti at them because they’re walking a hard road and their newfound parenthood is so worth celebrating.
Every life, no matter how small, no matter the circumstances, even the briefest, deserves to be recognized. So, never be discouraged to say, “Congratulations!”
Day Eight:
I want to switch gears a bit today and talk not about preemies, but nurses. Nurses are so critical to our babies' care when they are in the NICU and beyond. The expertise and compassion they have is immeasurable. I felt so comfortable knowing that Flynn was just where he needed to be and receiving the best care. As parents who were able to be by Flynn’s side a majority of the time, we built relationships with his care team and they became a part of our forever family.
The thing I remember the most is when I received absolute unnecessary and unexpected kindness. I want to tell you a story:
The night before my scheduled c-section and the same day, we found out that our baby was coming three months early. I connected to monitors, IVs, and compression machines. If I had to go to the bathroom - which I did quite frequently with all of that fluid I received, I had to unhook myself and hook my wires back up to a portable version of a similar setup. I could handle it, “Grey’s Anatomy” is kinda my thing, but the “getting up without hurting myself” was something I hadn’t mastered, especially amidst exhaustion.
I was lucky enough and very grateful to have my husband by my side the whole time, but he is a very sound sleeper, and he was very sleep-deprived. Despite my efforts, I couldn’t wake him up and gave it my best shot on my own. Wouldn’t you know it, though, I made it to the bathroom but got stuck coming back and had to use my portable call button to help me.
The nurse not only assured me that it was okay and this wasn’t the lowest of low points in my life, but she also helped me back into bed and asked the million-dollar question, “How are you doing?” And out came the tears, the grief, and sniffly (barely understandable) words of fear. But, instead of regretting that she ever asked the question, she rubbed my back and told me that it would all be okay until I fell asleep.
This woman, who has the knowledge and abilities to save people from dying, took the time out of her who-ever-knows-how-long shift to sit with a broken girl who was afraid, and I will always be thankful for her.
She checked on me after my c-section, even though I wasn’t her patient; when she found out I landed back in the ICU, you bet she visited then, too.
I could go on forever about nurses. Thank the nurses in your life. The world needs more people like them.
Day Nine:
In addition to being classified by gestational age, which I discussed on day three, premature babies are grouped based on their birth weight in grams, which the NICU uses as the unit of measure for weight. The classifications are: Low Birth Weight (LBW) - less than 2500 grams, Very Low Birth Weight (VLBW) - less than 1500 grams, Extremely Low Birth Weight (ELBW) - less than 1000 grams.
Flynn was born weighing 2lbs, 3oz, which is about 990 grams, placing him in the ELBW category. In his first few days, his weight decreased to 1lb, 15oz, which was pretty scary for us, even though this is pretty typical of babies born at any gestation, and it’s mostly water weight.
It’s hard to put into words how small a two-pound baby truly is. To me, he felt weightless and I could support both his head and bottom in the same hand. His head easily fit in my palm, his bottom on three of my fingers, his whole foot was no bigger than the tip of my thumb, and his tiny hand wrapped just about halfway around my pinky. This may not mean much to you, without knowing how big my hands and fingers are and it’s likely difficult to comprehend.
But, next time you’re holding a liter of Coke (or Pepsi or water) take a minute to think about the weight and know that Flynn weighed less than the bottle you’re lifting with ease. A human was so tiny, that a bottled beverage weighed more. If you haven’t been there, take a moment to imagine that.
Day Ten:
One of my first struggles with sadness as a preemie mom was curating a birth announcement. As silly as it sounds, for some, this is a Pinterest-worthy milestone moment, almost a rite of passage into motherhood in the new age.
“Look at my sweet baby! Look! I’m so excited that they’re here! Celebrate with me!”
Even at 28 weeks pregnant, I had a coming home/announcement outfit picked out. I remember after our first ultrasound, my husband and I went to Target to start our registry and saw the perfect grey onesie that said, “Hi, I’m new here!” and I knew that was THE outfit.
But, my baby was born too tiny, too fragile to wear clothing. It would be weeks before I could dress him, and even then, the wires and tubes wouldn’t allow for specific outfits. His first public photo was just his little foot, with his ankle bracelet smaller than my wedding ring, filtered in black and white, and cropped so the audience would see as little of his translucent skin and lifelines as possible. I didn’t want the first impression people had of our child to be that of pity. He was strong. We knew this.
It wasn’t the dream announcement that I had hoped, but I needed the support of people within our community.
After Flynn was discharged from the NICU and we approached his would-have-been birthday, we decided to have a newborn session with an amazing photographer who encouraged us to put him in the outfit we had chosen for him so many months ago. It was big for his small frame, but workable. Flynn didn’t love it, but I got my announcement photo - we just happened to choose a more content version of him (not wearing clothes, by the way) peering over the side of a basket. We still have it hanging on our wall. The point is, you can grieve and you can survive all Your expectations may need to change, but you can still get your “special.”
Day Eleven:
The experience that parents face when they have a child in the NICU can last long after discharged. Years later, the beep of a monitor or the smell of hospital soap can still take them back to those anxiety-ridden days in the NICU when they lived under the constant threat of losing their baby. These memories can often present as post-traumatic stress disorder (PTSD).
PTSD is a mental health condition that can develop after a person has experienced or witnessed a traumatic or terrifying event.
According to research, up to 53% of mothers and 33% of fathers with babies in the NICU suffer from PTSD. They discovered that mothers were more symptomatic earlier, but fathers had higher rates of post-traumatic stress months later when the child was home from the NICU.
PTSD can cause various symptoms including recurrent distressing memories, nightmares, flashbacks, intense distress or physical reactions to memory triggers, negative changes in mood and thinking, or changes in emotional reactions. Parents may haunted by flashbacks to their time spent in the NICU when their child gets sick, goes to a hospital for a routine procedure, or even on their birthday. Some of the signs and symptoms to meet criteria for PTSD can also be symptoms of other behavioral health disorders, so it is important to talk to a health care professional.
If this sounds like you, you are not alone. Help is available.
Day Twelve:
Did you know that preemies are sometimes called Million Dollar Babies?
The average cost of NICU care in the United States exceeds $3,000 per day. These costs do not include specialists that come to care for your child, special tests, or any surgeries/procedures needed. According to the March of Dimes, the average NICU stay is 13.2 days so when all is said and done, NICU bills can be pretty expensive!
With a lengthier or more complicated NICU stay, like Flynn’s, by the time a baby discharged, the total of all medical bills is potentially millions of dollars. There is also the cost of dozens of doctors and specialists visits on the calendar at any given time post-discharge, any medications or supplements prescribed, or any medical equipment. Sometimes, too, work circumstances must change so that your child can have the necessary, round-the-clock care that they need. Oh, and kids, in general, are just expensive!
Preemie parents scrounge, pinch pennies, get creative, and do whatever we can to stay afloat. We may choose to decline invitations to activities which involve spending money, even if it’s just the cost of gas. It’s tough, but we try our very best for our million-dollar babies.
Day Thirteen:
Today is World Kindness Day, so let’s talk about some ways to show your favorite preemie families that you love them!
1. Reach out to them, even if you have to leave a message, and ask how they’re doing.
2. If they are in isolation, stop by with coffee (or their beverage of choice) to drop off. Let them know it’s on their doorstep and that you’re thinking of them or that you’re outside if they want to talk - even if it’s through the door.
3. If their baby is still in the NICU, make sure you’re asking questions, just as you would any other new parent. And ask to see pictures because we love to show off our kids, too, tubes, wires, and all!
4. Keep in mind these parents are experiencing (or have experienced) a lot of trauma and that changes a person, even temporarily. If they open up to you, listen with compassion.
5. Don’t ask “if” you can help, but ask “how.” If they are a current NICU family, plan a meal train so they’ll be able to eat something. If they are managing several appointments or therapies, see if you can help with housework or watch siblings. Maybe even see how you can help so they can rest for an hour.
If you’re a preemie parent, how have you been shown kindness, either during your NICU stay or post-discharge?
Day Fourteen:
Today’s “lesson” is simple.
A premature baby is far smaller than you could ever imagine. Seeing a human that fits in just one of your hands is surreal, and those who have never held a preemie in real life may not be able to comprehend how little and weightless they can be.
Here is one of Flynn’s hands, at age three-and-a-half, next to one of his first outfits, just for a size comparison. At one point, he was far too small to fit in these tiny clothes, which is pretty unbelievable.
Day Fifteen:
When can the baby go home?
I strongly encourage loved ones of preemie families not to ask this question. The discharge of a preemie from the hospital isn't a single event, but a process. It’s a longer process for some than others and the truth is that there is no way of knowing when discharge day will be. There is a whole checklist of items that must be complete before a baby can go home. One of those items is the car seat test, where the baby is placed in the seat and attached to a monitor that evaluates the heart and breathing.
A preemie often does not have the muscle control needed to keep their head upright or move it if they have trouble breathing. Many car seats even need to be modified by the NICU so that the baby’s head stays in a position that keeps the airway open. Often it is recommended that parents limit car seat time to only an hour. Some babies have respiratory conditions that prevent them from traveling in a traditional infant car seat, and they must use a unique restraint system.
I’ll never forget that first ride home. Flynn was still so unbelievably tiny at just four pounds, and seeing him in the outside world made him look even smaller. I’d never been so panicked as I was in that car that day and was so relieved when we pulled into the driveway. Most parents probably worry about the dangers of being in a car, but I was so nervous that he would stop breathing. We finally made it home.
Day Sixteen:
For the longest time, I had a breast pump under my bed, collecting dust. It’s was never used and it hurt my heart to look at it. I genuinely believe that “fed is best,” but my personal goal was to breastfeed for as long as I could. Our baby registry was filled with breast pumps, carrying cases, special bottles that simulated the breast, pads, and nipple cream (which I’d heard was a cure-all). I was all in, well, as much as I could be without an actual baby to feed. Then, Flynn was born three months early.
When a baby is born prematurely, they may not yet have the ability to coordinate their sucking, swallowing, and breathing and cannot take food directly from a bottle or breast. This usually develops around 34 weeks, but they can receive breast milk or formula through their feeding tube. So, right away, I started working on developing my milk supply by pumping with a hospital-provided breast pump. And when I say “right away,” I mean in the recovery room directly post-surgery. My husband and sister met Flynn for the first time, and I met with a lactation consultant. In my mind, I couldn’t do much for him but I could do this.
Milk production begins around the midpoint of pregnancy. For most mothers, milk will increase in quantity and begin the change from colostrum to mature milk between days two and five. The thing about prematurity is, your body still thinks you are pregnant even after the baby has arrived. So, this makes the process of breastfeeding/pumping extremely difficult. I pumped for an hour, every three hours, around the clock, and my husband would deliver it to the NICU. After we went home, we collected the supply and brought it to Flynn when we visited each day. When I was in the ICU, I pumped what I could but had to throw away a lot of it due to my medications. I kept going because I did not want to lose the supply that I had. I signed some paperwork so that Flynn could receive milk from an anonymous donor from the hospital’s “milk bank” to supplement my supply. The milk was screened and sterilized and given from approved donors to babies who needed it.
After all of that, my body quit on me. I tried until I was bleeding and raw, but I couldn’t do it and I felt like a failure, once again. Yet, I couldn’t seem to get rid of that breast pump until this year...
Thank you for reading, if you would like to follow Kristina check out her Instagram at @oneinamulligan or her blog at https://www.oneinamulligan.com/

Cressie